You’re reading the web edition of STAT’s Health Tech newsletter, our guide to how technology is transforming the life sciences. Sign up to get it delivered in your inbox every Tuesday and Thursday.
Oracle reveals ‘AI’ electronic health record software
Oracle Health this week began previewing its “next-generation” electronic health record software “powered by AI” that it claims was “built from the ground up” and features “military grade security.” Given rates of adoption of new things in health care, I was somewhat skeptical we would learn what any of that means in the near future, but the company says an early adopter program for the EHR will begin some time in 2025.
Oracle Health is the entity that arose from the tech giant’s acquisition of number two health record vendor Cerner several years ago. Like everyone in the space, it’s fighting a battle for market with the Epic Systems juggernaut, a company that has become so powerful that it’s facing allegations of antitrust violations.
And while its hard to suss out substance from PR noise at this point, I think many in health care would agree with the spirit of Oracle’s effort to refresh health records technology. At this point, clinicians complaining about unwieldy, outmoded software they must use for hours each day is a tired joke. If Oracle’s alternative feels more like the slick software we use everywhere else in our lives, then maybe it can find some buyers.
Related: Earlier this year, in the spring, my colleague Mohana Ravindranath talked to Oracle Health chairman David Feinberg.
Talkspace’s Medicare progress, Teladoc’s BetterHelp slump, Amwell’s big hire
Quarterly earnings season has finally come to the world of telehealth. A few high-level takeaways:
Several months after replacing its CEO, Teladoc is still figuring it out. The company’s third quarter revenues declined year over year — but they declined less than investors said they would. BetterHelp, Teladoc’s direct-to-consumer mental health business, continued to shrink, despite advertising on all your favorite podcasts. Indeed, BetterHelp’s advertising spend continues to be a drag on the company’s margins. Elsewhere, the company is making small gains on its integrated care business but suggested buyers were hesitant to pick up new services right now.
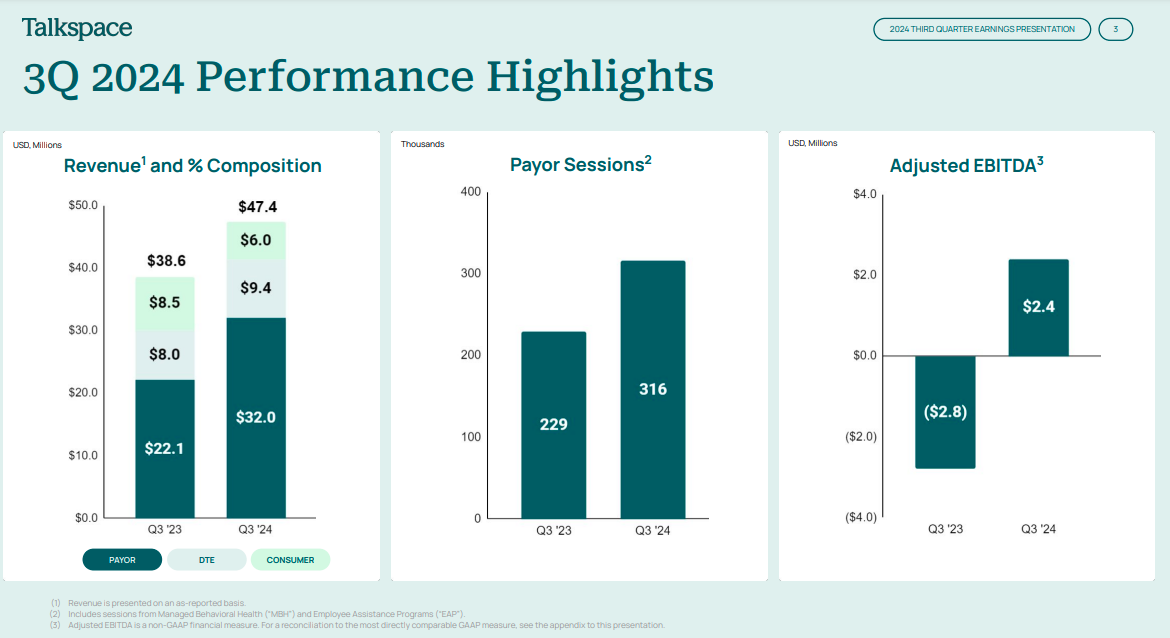
Virtual mental health company Talkspace continued its streak as one of the bright spots in virtual care business, posting increasing revenues and looking more and more like it might be a sustainable business in the long term. The company’s strategy for several years has been to grow the number of people who use its services through health plans and other coverage as opposed to paying out of pocket. Given BetterHelp’s direct-to-consumer struggles (see above) that push seems prescient. Earlier this year the company announced an expansion into Medicare, which is now live in 30 states, and the company has added Medicare Advantage plans as well. Talkspace said it’s targeting 200 million covered lives next year.
Elsewhere, virtual care provider and infrastructure company Amwell knocked down its guidance range from $259—$269 million to $247—$252 million, reaffirming investor fears about the company’s long-term path to break-even. The company has made progress rolling out its key large contract with the Defense Health Agency, but elsewhere it is seeing declining use of its medical group services. Amwell lowered its projection for number of visits this year. In fairness, the company also reduced its projection for how much money it would lose on an adjusted basis.
Of note: Amwell announced it hired veteran health tech executive Mark Hirschhorn as chief financial officer. Hirschhorn most recently was CEO at Tapestry Health, but is better known for previous chief operating officer roles at Teladoc and Talkspace. But close observers might remember that those relationships both ended on acrimonious terms, as I reported at the time.
What to know about Apple’s hearing health push
Apple this week officially released a batch of new health features for AirPods Pro that allow users to test their hearing and use the popular wireless headphones as hearing aids for milder forms of hearing loss.
Even before the release, Apple’s hearing health features were praised by audiologists and other experts for their potential to help more people address hearing loss. But as I write in a new story, the company’s technologies, which blur the line between consumer feature and medical device, don’t fit neatly into the traditional world of hearing care. The company claims, for example, that its hearing aid software is “clinical grade” a term that doesn’t have a definition. It might be interpreted as a nod to the feature’s FDA marketing authorization (true!) or to suggest the product is as good as prescription hearing aids audiologists recommend (not true!).
I spoke to hearing experts as well as Apple executives who explained the ins and outs of how the features work and what we ought to know about them. Read more here
5 investors driving health tech’s biggest deals
There’s been a rash of recent big funding deals in health tech, stoking optimism that investors may be warming up. So who’s writing the big checks? STAT’s Mohana Ravindranath profiled five of the names behind significant deals, including Bryan Roberts from Venrock, which recently backed AI clinical note company Suki, and Nancy Brown from Oak HC/FT who recently led a a $60 million investment in digestive care company Oshi Health. Read more about the folks behind some of the biggest recent health tech deals.
A prominent call to revise use of race in research
Remember the series of stories my colleagues Katie Palmer and Usha Lee McFarling did on the use of race as a factor in clinical algorithms that doctors use everyday in health care settings to make decisions about patients care? As their reporting revealed, these algorithms could perpetuate health disparities because of the way race, a social construct, is used. The challenge is removing them might also lead to harm. But, there is some hope for change on the horizon.
On Wednesday, the National Academies of Science, Engineering, and Medicine issued a new report that called on scientists, research funders, and publishers to transform the way they use — and don’t use — race and ethnicity in biomedical research. The report addressed clinical algorithms and said simply removing race from them would not resolve issues, but recommended that new tools be developed with more transparency and have their performance reported across different racial and ethnic groups. It noted that such calculators were based on biomedical research that often had deeply rooted bias. Developers of those tools often “start to point fingers downstream at the people who are collecting data, and then the researchers who are publishing the data,” said Shazia Siddique, a health systems researcher and gastroenterologist at the University of Pennsylvania who led a review by the Agency for Healthcare Research and Quality on the impact of health care algorithms on racial and ethnic disparities. “Ultimately, I think it takes all of us to make change.”
Read about the new National Academies report here, and dive into STAT’s previous reporting on the issue in the Embedded Bias series.
What we’re reading
- UnitedHealth Group names new CISO 8 months after massive ransomware attack, Cybersecurity Dive
- Global summit blends AI and biotech, Axios
- Should race be used in clinical algorithms? How one doctor’s research is helping shape policy, STAT