Detecting tumor infiltration during surgery has been a vital concern for over a century. Despite advances in healthcare, the issue of residual tumors remains a significant challenge, particularly in the context of brain and solid cancers.
Residual tumor tissue, left behind after surgery, can worsen a patient’s prognosis, reduce quality of life, and strain healthcare systems. This problem has persisted for decades, with corrective surgeries and follow-up treatments costing over $1 billion annually in the United States.
Unlike traditional methods, this tool provides real-time diagnostic insights during surgery, enabling precise tumor resection within seconds.
Dr. Todd Hollon, a neurosurgeon and assistant professor at the University of Michigan Medical School, explains, “FastGlioma is an artificial intelligence-based diagnostic system that has the potential to change the field of neurosurgery by immediately improving comprehensive management of patients with diffuse gliomas.”
By identifying tumor infiltration quickly and accurately, this technology minimizes the risk of leaving residual tumor tissue behind.
Residual tumors often go unnoticed during surgery because their appearance can closely mimic that of healthy brain tissue. Surgeons rely on several tools to locate residual tumors, including MRI imaging and fluorescent agents. However, these methods are not universally available and may not work for all tumor types.
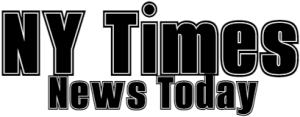
FastGlioma addresses these limitations by combining advanced optical microscopy with foundation AI models trained on extensive datasets.
This AI system leverages stimulated Raman histology, a rapid and high-resolution imaging method, to analyze fresh, unprocessed surgical specimens. By doing so, FastGlioma can detect residual tumor tissue in as little as 10 seconds.
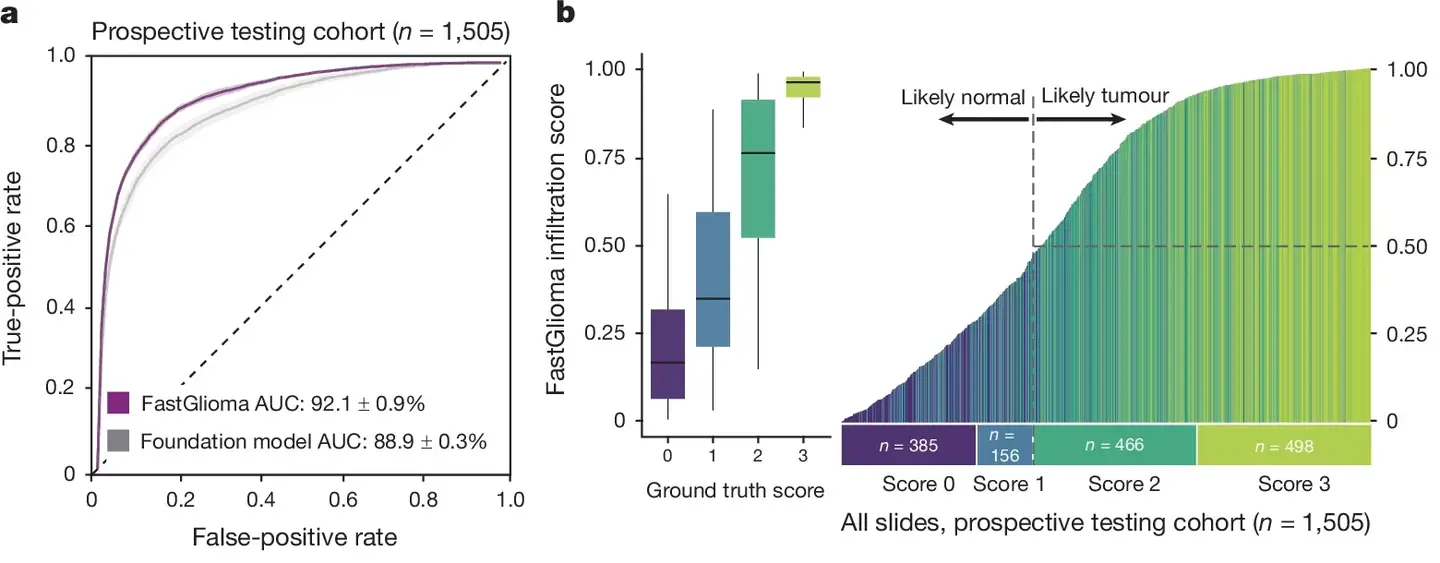
According to the study, published in Nature, the system achieved an impressive 92% accuracy in detecting tumor remnants, significantly outperforming conventional imaging and fluorescent methods.
“FastGlioma represents an innovative departure from existing surgical techniques by rapidly identifying tumor infiltration at microscopic resolution,” says Dr. Shawn Hervey-Jumper, a professor of neurosurgery at UCSF. The technology’s ability to detect tumor tissue without relying on time-consuming histology or expensive imaging tools makes it a game-changer, especially in resource-limited settings.
The accuracy of FastGlioma is further demonstrated by its ability to minimize high-risk residual tumor cases. Traditional methods miss residual tumor tissue nearly 25% of the time, while FastGlioma reduces this miss rate to just 3.8%. This significant improvement could lead to better surgical outcomes, lower recurrence rates, and improved patient survival.
FastGlioma’s underlying technology draws from visual foundation models similar to GPT-4 and DALL-E, known for their adaptability across various tasks.
These models were trained on over 11,000 surgical specimens and 4 million unique microscopic fields of view, allowing FastGlioma to generalize across diverse patient populations and healthcare environments. Its user-friendly interface provides neurosurgeons with immediate, actionable insights, enhancing their decision-making process during operations.
This system’s potential extends beyond gliomas. Researchers believe it could be adapted to detect other types of brain tumors, including pediatric tumors like medulloblastoma and ependymoma, as well as meningiomas.
Dr. Aditya S. Pandey, chair of the Department of Neurosurgery at U-M Health, states, “These results demonstrate the advantage of visual foundation models such as FastGlioma for medical AI applications and the potential to generalize to other human cancers without requiring extensive model retraining.”
The implications of this technology are profound, particularly in addressing the global burden of cancer surgery. The Lancet Oncology Commission emphasized the need for innovative approaches to improve surgical margins in cancer treatment. FastGlioma aligns perfectly with this vision, offering a cost-effective and accessible solution that can enhance surgical precision worldwide.
Looking ahead, the research team aims to expand FastGlioma’s applications to other cancer types, including lung, prostate, breast, and head and neck cancers. If successful, this could mark a new era in surgical oncology, where AI-driven tools play a central role in improving patient outcomes and reducing healthcare costs.
FastGlioma’s rapid, accurate, and scalable approach represents a significant leap forward in the fight against cancer. By integrating cutting-edge AI with practical surgical tools, this technology offers hope for better outcomes and a higher quality of life for patients facing one of the most challenging diagnoses.